A System Rigged Against the Little Guy
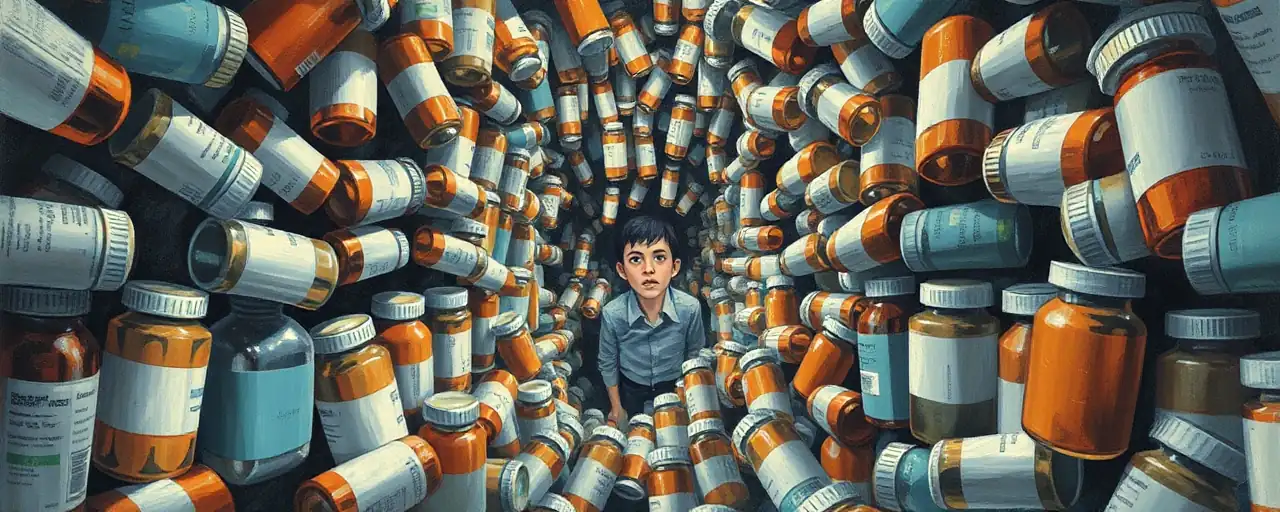
Walk into any small-town pharmacy, and you’ll see it: shelves stocked with care, a pharmacist who knows your name, and a community hub hanging on by a thread. These independent pharmacies, once the backbone of American healthcare, are vanishing. The culprit isn’t just market forces; it’s a shadowy middleman called the Pharmacy Benefit Manager, or PBM. These corporate giants, meant to streamline drug costs, have instead ballooned into profit-hungry behemoths that choke local businesses and drive up prices for everyone.
California Attorney General Rob Bonta, alongside 38 other state attorneys general, recently sounded the alarm. In a bold letter to Congress, they demanded a federal law to stop PBMs, their parent companies, or affiliates from owning pharmacies. Their reasoning is simple yet urgent: PBMs have gamed the system, consolidating power to favor their own profits over patients and small businesses. This isn’t just a policy issue; it’s a moral failing that leaves rural families stranded and urban communities underserved.
The numbers tell a grim story. Over the last decade, nearly 39% of independent pharmacies shuttered, compared to just 22% of chain stores. In rural areas, one in ten independent pharmacies closed, creating pharmacy deserts where people must travel miles for a prescription. This isn’t progress; it’s a betrayal of the promise that healthcare should reach everyone, no matter where they live.
The PBM Power Grab
PBMs started in the 1960s with a noble goal: help insurers manage drug benefits and keep costs down. Fast forward to 2025, and the top three—CVS Caremark, OptumRx, and Express Scripts—control 80% of prescriptions nationwide. They’ve morphed from helpers to overlords, using their clout to manipulate prices and squeeze out competition. How? Through vertical integration, where PBMs own pharmacies, insurers, and even clinics, creating a closed loop that locks out independent players.
Take spread pricing, a tactic where PBMs charge insurers more than they pay pharmacies, pocketing the difference. The Federal Trade Commission found PBMs raked in over $7.3 billion in excess revenue from specialty generics alone between 2017 and 2022. Then there’s rebate retention, where PBMs keep a chunk of manufacturer discounts instead of passing savings to patients. These practices aren’t just unfair; they’re a direct hit on families already struggling to afford medications.
Independent pharmacists face the brunt. PBMs set reimbursement rates so low that many operate at a loss. In Alabama, dozens of pharmacies closed in the past two years, unable to survive PBMs’ take-it-or-leave-it contracts. Kansas saw over 100 pharmacies shutter temporarily in early 2025, a desperate protest against terms that favor PBM-owned chains. Meanwhile, patients, especially in Black and Latino neighborhoods, lose access to trusted local care as closures hit hardest there.
The Myth of Market Efficiency
Some defend PBMs, claiming their size brings efficiency and lower costs. They argue PBMs negotiate discounts that benefit insurers and promote generics to save money. But this is a half-truth at best. While PBMs secure rebates, patients rarely see the savings. Instead, 30% of Americans report struggling to afford prescriptions, and over 20% have skipped doses due to cost. If this is efficiency, it’s working for corporate bottom lines, not people.
The idea that PBMs foster competition is even harder to swallow. Their ownership of pharmacies lets them steer patients to their own stores, sidelining independents. The American Medical Association found 72% of people with commercial or Medicare Part D plans are tied to insurers linked with PBMs. This isn’t a free market; it’s a rigged game where PBMs hold all the cards, and small pharmacies are forced to fold.
Supporters of the status quo often point to programs that claim to help rural pharmacies. Yet these initiatives are bandages on a gaping wound. When reimbursement rates don’t cover costs, and contracts come with arbitrary terms, no program can undo the damage of a system that prioritizes profit over access.
A Call for Justice
The bipartisan push led by Bonta offers a lifeline. Banning PBMs from owning pharmacies would level the playing field, forcing them to compete fairly rather than strong-arm competitors. States like Alabama and Iowa have already taken steps, passing laws to curb spread pricing and protect local pharmacies. But patchwork state fixes aren’t enough. Federal action is critical to dismantle a system that’s grown too big, too fast.
This fight is about more than pharmacies; it’s about who gets to thrive in America. Every closed pharmacy means fewer jobs, less access, and weaker communities. It’s time for Congress to act, to prove that healthcare isn’t just for the powerful. A law breaking PBMs’ grip would send a clear message: no corporation gets to profit by leaving people behind.